Inhalation of hydrogen gas after myocardial infarctionScientific Research

The Effects of Hydrogen Gas Inhalation on Adverse Left Ventricular Remodeling After Percutaneous Coronary Intervention for ST-Elevated Myocardial Infarction ― First Pilot Study in Humans ―
Abstract
Abstract
Background: In a rat model of acute myocardial infarction (AMI), hydrogen gas (HI) inhalation reduces infarct size and attenuates unnecessary left ventricular (LV) remodeling. We designed a prospective, open-label, rater-blind clinical study of patients with ST-segment elevation myocardial infarction (STEMI).
METHODS AND RESULTS
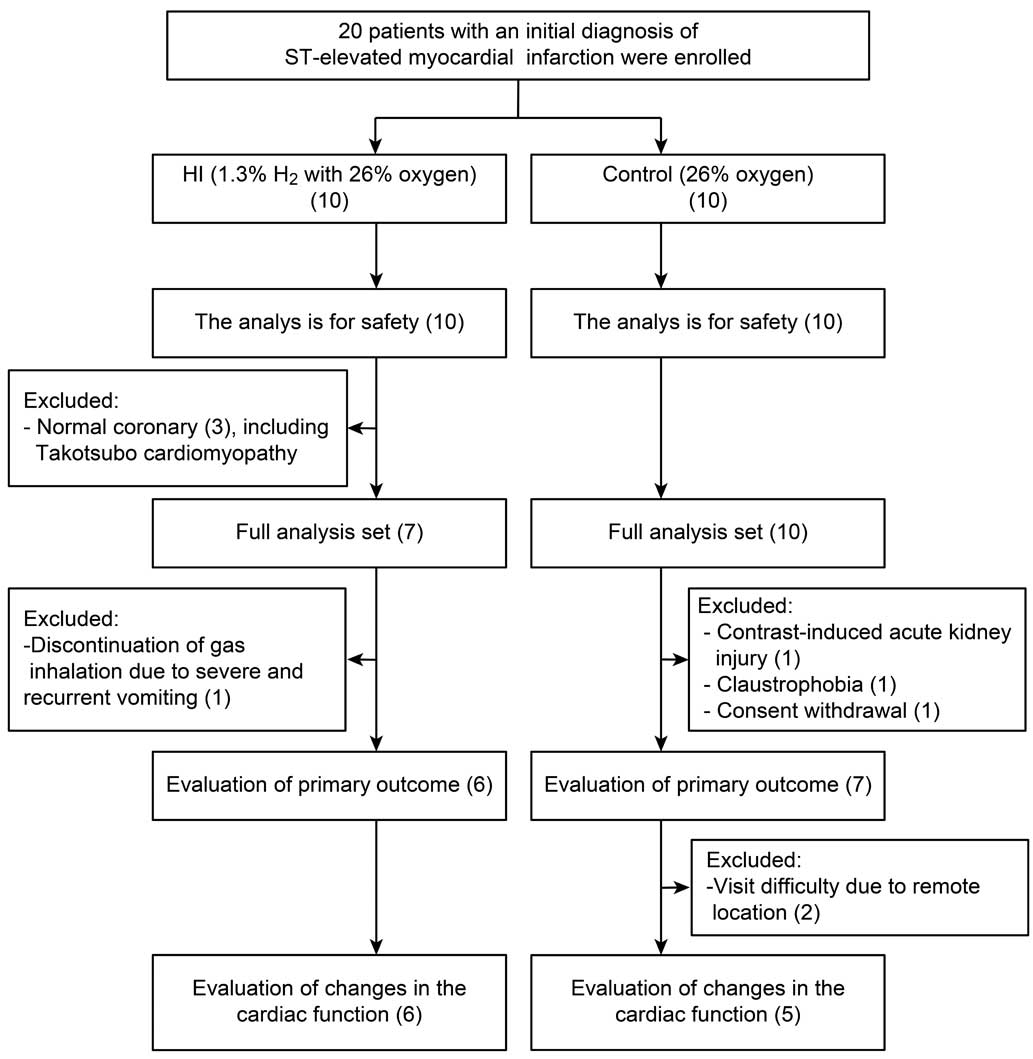
Twenty patients with an initial diagnosis of STEMI were assigned to either the HI group (1.3% H2 and 26% oxygen) or the control group (26% oxygen).
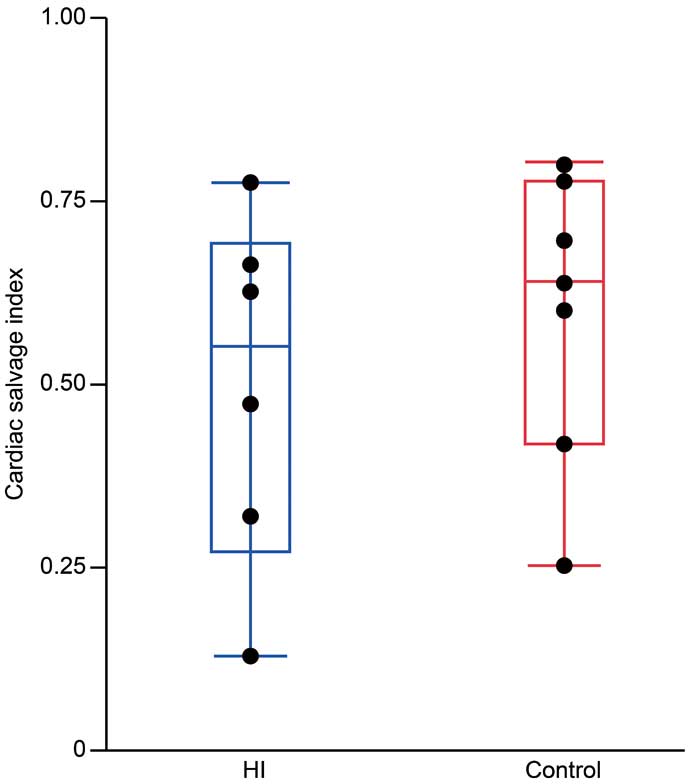
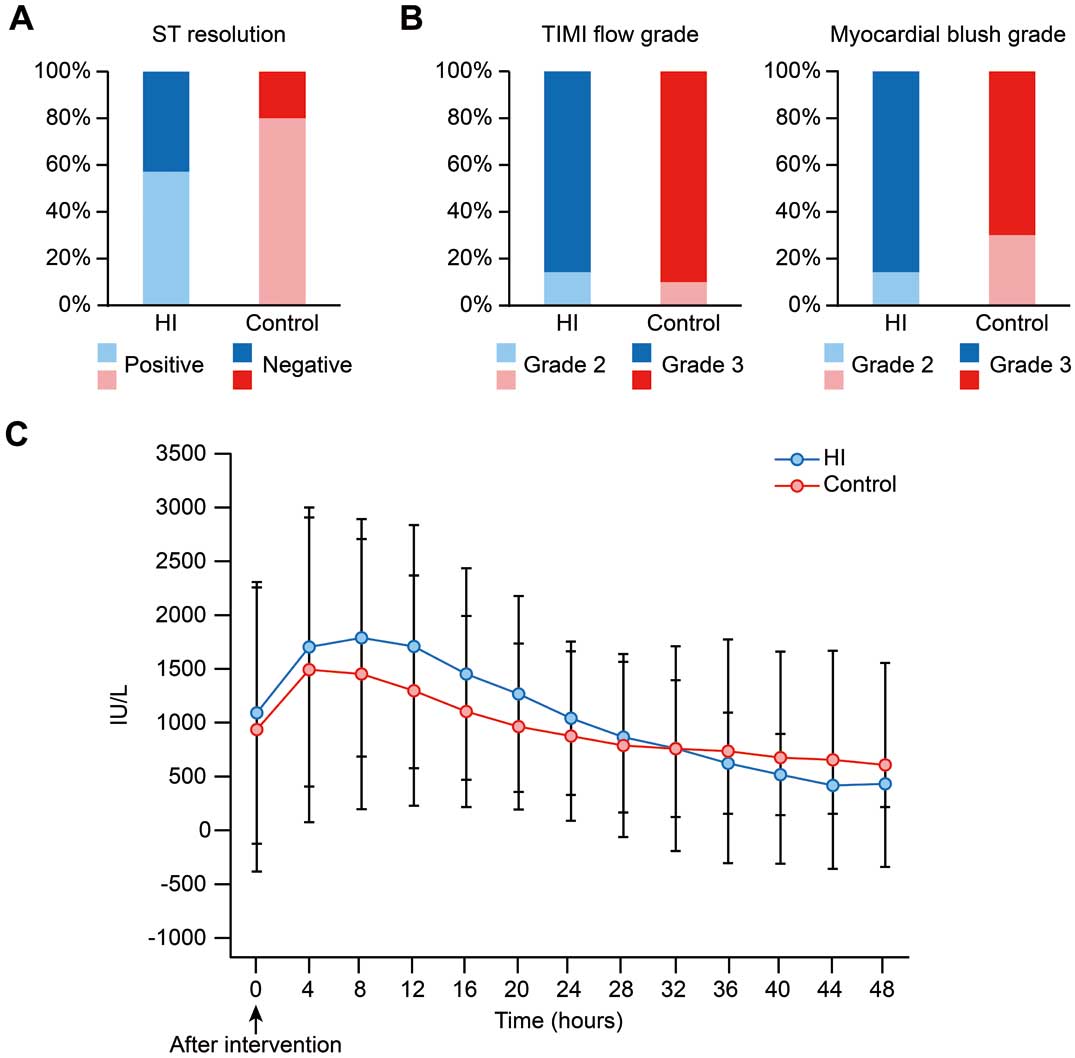
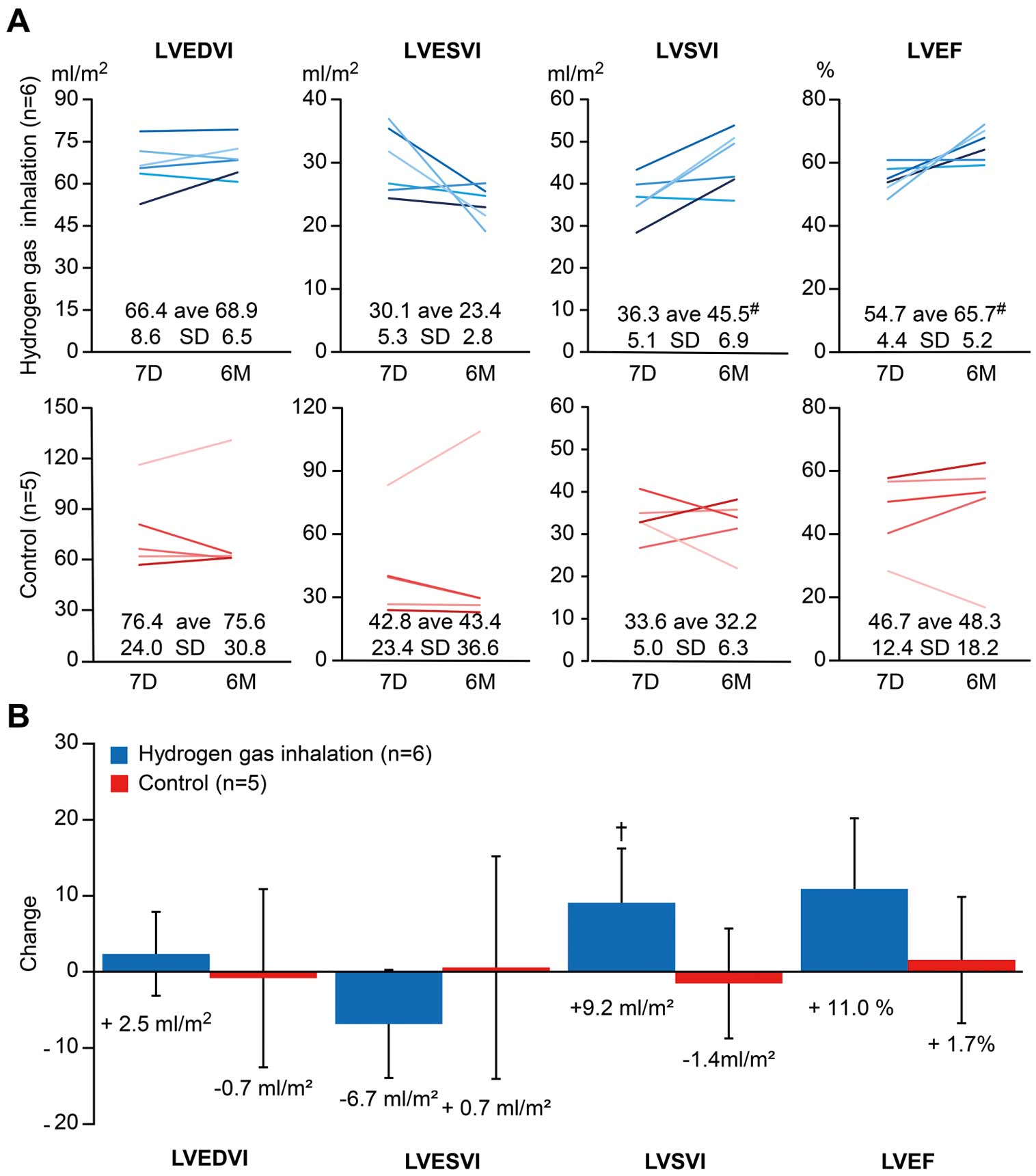
There were no serious adverse events related to HI. In the entire analysis set, the cardiac salvage index assessed by cardiac magnetic resonance imaging 7 days after primary percutaneous coronary intervention (PCI) showed no significant difference between the two groups (HI: 50.0 ± 24.3%; control group: 60.1 ± 20.1%; P = 0.43). However, at 6 months, some surrogate outcomes from day 7 were numerically greater in the HI group than in the control group, including the LV stroke volume index (HI: 9.2 ± 7.1 mL/m2; control: -1.4 ± 7.2 ml /m2; P = 0.03) and LV ejection fraction (HI: 11.0% ± 9.3%; control: 1.7% ± 8.3%; P = 0,11).
Conclusions
The first clinical study demonstrated that HI during PCI is feasible and safe, promoting reverse LV remodeling even 6 months after STEMI. The study was not designed to test efficacy, and another large-scale study is needed. (Clinical trial registration number: UMIN00006825)
References
- 7. Ohta S. Molecular hydrogen as a novel antioxidant: Overview of the advantages of hydrogen for medical applications. Methods Enzymol 2015; 555: 289–317.
- 12. Homma K, Yoshida T, Yamashita M, Hayashida K, Hayashi M, Hori S. Inhalation of hydrogen gas is beneficial for preventing contrast-induced acute kidney injury in rats. Nephron Exp Nephrol 2014; 128: 116–122.
- 14. Yoshida A, Asanuma H, Sasaki H, Sanada S, Yamazaki S, Asano Y, et al. H(2) mediates cardioprotection via involvements of K(ATP) channels and permeability transition pores of mitochondria in dogs. Cardiovasc Drugs Ther 2012; 26: 217–226.
- 16. Masci PG, Ganame J, Strata E, Desmet W, Aquaro GD, Dymarkowski S, et al. Myocardial salvage by CMR correlates with LV remodeling and early ST-segment resolution in acute myocardial infarction. JACC Cardiovasc Imaging 2010; 3: 45–51.
- 17. Wright J, Adriaenssens T, Dymarkowski S, Desmet W, Bogaert J. Quantification of myocardial area at risk with T2-weighted CMR: Comparison with contrast-enhanced CMR and coronary angiography. JACC Cardiovasc Imaging 2009; 2: 825–831.
- 20. Smith DH, Neutel JM, Lacourciere Y, Kempthorne-Rawson J. Prospective, randomized, open-label, blinded-endpoint (PROBE) designed trials yield the same results as double-blind, placebo-controlled trials with respect to ABPM measurements. J Hypertens 2003; 21: 1291–1298.
- 23. Yan X, Shichita T, Katsumata Y, Matsuhashi T, Ito H, Ito K, et al. Deleterious effect of the IL-23/IL-17A axis and gammadeltaT cells on left ventricular remodeling after myocardial infarction. J Am Heart Assoc 2012; 1: e004408.
- 25. Yan X, Hegab AE, Endo J, Anzai A, Matsuhashi T, Katsumata Y, et al. Lung natural killer cells play a major counter-regulatory role in pulmonary vascular hyperpermeability after myocardial infarction. Circ Res 2014; 114: 637–649.
- 26. Katsumata Y, Shinmura K, Sugiura Y, Tohyama S, Matsuhashi T, Ito H, et al. Endogenous prostaglandin D2 and its metabolites protect the heart against ischemia-reperfusion injury by activating Nrf2. Hypertension 2014; 63: 80–87.
- 27. Sugiura Y, Katsumata Y, Sano M, Honda K, Kajimura M, Fukuda K, et al. Visualization of in vivo metabolic flows reveals accelerated utilization of glucose and lactate in penumbra of ischemic heart. Sci Rep 2016; 6: 32361.
The Effects of Hydrogen Gas Inhalation on Adverse Left Ventricular Remodeling After Percutaneous Coronary Intervention for ST-Elevated Myocardial Infarction ― First Pilot Study in Humans ―
Abstract
Abstract
Background: In a rat model of acute myocardial infarction (AMI), hydrogen gas (HI) inhalation reduces infarct size and attenuates unnecessary left ventricular (LV) remodeling. We designed a prospective, open-label, rater-blind clinical study of patients with ST-segment elevation myocardial infarction (STEMI).METHODS AND RESULTS
Twenty patients with an initial diagnosis of STEMI were assigned to either the HI group (1.3% H2 and 26% oxygen) or the control group (26% oxygen).
There were no serious adverse events related to HI. In the entire analysis set, the cardiac salvage index assessed by cardiac magnetic resonance imaging 7 days after primary percutaneous coronary intervention (PCI) showed no significant difference between the two groups (HI: 50.0 ± 24.3%; control group: 60.1 ± 20.1%; P = 0.43). However, at 6 months, some surrogate outcomes from day 7 were numerically greater in the HI group than in the control group, including the LV stroke volume index (HI: 9.2 ± 7.1 mL/m2; control: -1.4 ± 7.2 ml /m2; P = 0.03) and LV ejection fraction (HI: 11.0% ± 9.3%; control: 1.7% ± 8.3%; P = 0,11).
Conclusions
The first clinical study demonstrated that HI during PCI is feasible and safe, promoting reverse LV remodeling even 6 months after STEMI. The study was not designed to test efficacy, and another large-scale study is needed. (Clinical trial registration number: UMIN00006825)
References
- 7. Ohta S. Molecular hydrogen as a novel antioxidant: Overview of the advantages of hydrogen for medical applications. Methods Enzymol 2015; 555: 289–317.
- 12. Homma K, Yoshida T, Yamashita M, Hayashida K, Hayashi M, Hori S. Inhalation of hydrogen gas is beneficial for preventing contrast-induced acute kidney injury in rats. Nephron Exp Nephrol 2014; 128: 116–122.
- 14. Yoshida A, Asanuma H, Sasaki H, Sanada S, Yamazaki S, Asano Y, et al. H(2) mediates cardioprotection via involvements of K(ATP) channels and permeability transition pores of mitochondria in dogs. Cardiovasc Drugs Ther 2012; 26: 217–226.
- 16. Masci PG, Ganame J, Strata E, Desmet W, Aquaro GD, Dymarkowski S, et al. Myocardial salvage by CMR correlates with LV remodeling and early ST-segment resolution in acute myocardial infarction. JACC Cardiovasc Imaging 2010; 3: 45–51.
- 17. Wright J, Adriaenssens T, Dymarkowski S, Desmet W, Bogaert J. Quantification of myocardial area at risk with T2-weighted CMR: Comparison with contrast-enhanced CMR and coronary angiography. JACC Cardiovasc Imaging 2009; 2: 825–831.
- 20. Smith DH, Neutel JM, Lacourciere Y, Kempthorne-Rawson J. Prospective, randomized, open-label, blinded-endpoint (PROBE) designed trials yield the same results as double-blind, placebo-controlled trials with respect to ABPM measurements. J Hypertens 2003; 21: 1291–1298.
- 23. Yan X, Shichita T, Katsumata Y, Matsuhashi T, Ito H, Ito K, et al. Deleterious effect of the IL-23/IL-17A axis and gammadeltaT cells on left ventricular remodeling after myocardial infarction. J Am Heart Assoc 2012; 1: e004408.
- 25. Yan X, Hegab AE, Endo J, Anzai A, Matsuhashi T, Katsumata Y, et al. Lung natural killer cells play a major counter-regulatory role in pulmonary vascular hyperpermeability after myocardial infarction. Circ Res 2014; 114: 637–649.
- 26. Katsumata Y, Shinmura K, Sugiura Y, Tohyama S, Matsuhashi T, Ito H, et al. Endogenous prostaglandin D2 and its metabolites protect the heart against ischemia-reperfusion injury by activating Nrf2. Hypertension 2014; 63: 80–87.
- 27. Sugiura Y, Katsumata Y, Sano M, Honda K, Kajimura M, Fukuda K, et al. Visualization of in vivo metabolic flows reveals accelerated utilization of glucose and lactate in penumbra of ischemic heart. Sci Rep 2016; 6: 32361.



