Hydrogen Therapy in Colorectal Cancer TreatmentScientific Research
H2 gas rejuvenates CD8+ T cells in advanced colorectal cancer
Hydrogen inhalation may limit cancer progression and extend overall survival in advanced colorectal cancer patients. This is the conclusion of a medical study conducted with 21 men and 34 women at the Tamana Medical Health Center in Japan.
The study investigated the role of hydrogen in restoring exhausted immune cells that play a key role in fighting malignant tumors, both in colorectal and other cancers.
Patients were between the ages of 28 and 96 years old – diagnosed with stage 4 colorectal carcinoma. All 55 participants received conventional chemotherapy while also inhaling hydrogen for 3 hours each day at home. Hydrogen inhalation was carried out using a home hydrogen therapy device.
Patients signed written informed consent before enrolling in the study, and the study protocol was approved by the responsible institutional review boards. The methods and procedures followed Good Clinical Practice according to the Declaration of Helsinki and local laws.
Patient status was monitored at regular intervals with blood tests and CT or MRI scans. The scan results were reviewed by two independent radiologists who were deliberately blinded to the study topic to ensure maximum objectivity. Each radiologist has more than 5 years of experience in the interpretation of diagnostic imaging, which guaranteed their experience, professionalism, and objectivity.
At the end of the study, it was found that hydrogen significantly contributed to the restoration of the immune system and thus helped the body fight cancer cells effectively on its own. Additionally, none of the patients reported any problems as a result of hydrogen therapy. Similar results have been achieved in numerous other scientific studies investigating the benefits of hydrogen therapy in the fight against various cancers.
Thanks to this study, a system has been developed that can be useful in real clinical practice, helping healthcare professionals to determine more effective and personalized treatment methods based on individual patient characteristics.
Hydrogen therapy has shown impressive results and strong promise in the field of immunotherapy and may be the key to the future in the fight against cancer and healthcare as a whole.
This discovery opens up new possibilities for the treatment of colorectal cancer, especially in advanced stages where treatment options are often limited. Numerous other studies also suggest that in the future, cancer could be more easily treated with this innovative method.
The Original Article:
original title: Hydrogen gas restores exhausted CD8+ T cells in patients with advanced colorectal cancer to improve prognosis
DOI: 10.3892/or.2018.6841Published on: 2019
-
Abstract:
Exhausted cluster of differentiation (CD)8+ T cells lose immunological activity due to mitochondrial dysfunction caused by peroxisome proliferator‑activated receptor γ coactivator 1α (PGC‑1α) inactivation, resulting in a poor prognosis in patients with cancer. As hydrogen gas was recently reported to activate PGC‑1α, the present study investigated whether it restores exhausted CD8+ T cells to improve prognosis in patients with stage IV colorectal cancer. A total of 55 patients with histologically and clinically diagnosed stage IV colorectal carcinoma were enrolled between July 2014 and July 2017. The patients inhaled hydrogen gas for 3 h/day at their own homes and received chemotherapy at the Tamana Regional Health Medical Center (Tamana, Kumamoto, Japan). The CD8+ T cells were isolated from the peripheral blood and their phenotype was analyzed by flow cytometry. It was found that exhausted terminal programmed cell death 1 (PD‑1)+ CD8+ T cells in the peripheral blood are independently associated with worse progression‑free survival (PFS) and overall survival (OS). Notably, hydrogen gas decreased the abundance of exhausted terminal PD‑1+ CD8+ T cells, increased that of active terminal PD‑1‑ CD8+ T cells, and improved PFS and OS times, suggesting that the balance between terminal PD1+ and PD1‑ CD8+ T cells is critical for cancer prognosis. Therefore, a novel system for patient classification (category 1‑4) was developed in the present study based on these two indices to assist in predicting the prognosis and therapeutic response. Collectively, the present results suggested that hydrogen gas reverses imbalances toward PD‑1+ CD8+ T cells to provide an improved prognosis.
Hideo Baba, Junji Akagi
Original PublicationAbstract
Exhausted cluster of differentiation (CD)8+ T cells lose immunological activity due to mitochondrial dysfunction caused by peroxisome proliferator‑activated receptor γ coactivator 1α (PGC‑1α) inactivation, resulting in a poor prognosis in patients with cancer. As hydrogen gas was recently reported to activate PGC‑1α, the present study investigated whether it restores exhausted CD8+ T cells to improve prognosis in patients with stage IV colorectal cancer. A total of 55 patients with histologically and clinically diagnosed stage IV colorectal carcinoma were enrolled between July 2014 and July 2017. The patients inhaled hydrogen gas for 3 h/day at their own homes and received chemotherapy at the Tamana Regional Health Medical Center (Tamana, Kumamoto, Japan). The CD8+ T cells were isolated from the peripheral blood and their phenotype was analyzed by flow cytometry. It was found that exhausted terminal programmed cell death 1 (PD‑1)+ CD8+ T cells in the peripheral blood are independently associated with worse progression‑free survival (PFS) and overall survival (OS). Notably, hydrogen gas decreased the abundance of exhausted terminal PD‑1+ CD8+ T cells, increased that of active terminal PD‑1‑ CD8+ T cells, and improved PFS and OS times, suggesting that the balance between terminal PD1+ and PD1‑ CD8+ T cells is critical for cancer prognosis. Therefore, a novel system for patient classification (category 1‑4) was developed in the present study based on these two indices to assist in predicting the prognosis and therapeutic response. Collectively, the present results suggested that hydrogen gas reverses imbalances toward PD‑1+ CD8+ T cells to provide an improved prognosis.Introduction
In patients with cancer, the treatment strategy, outcome and prognosis are strongly dependent on immune status, which should thus be monitored, ideally via markers that are easily and non-invasively measurable in the peripheral blood. Cytotoxic effector cluster of differentiation (CD)8+ T cells (equivalent to terminal CD8+ T cells) become exhausted by persistent stimulation with tumor antigens, resulting in cessation of proliferation, cytokine production and immune activities (1,2). Programmed cell death 1 (PD-1) has been proposed as a marker of exhausted T cells (1). PD-1 is abundantly expressed in circulating CD8+ T cells in patients with cancer, as well as in tumor-infiltrating lymphocytes, and is associated with a poor prognosis in various cancer types, including breast, pancreatic and gastric cancer (3–6). As recently reported, exhausted tumor-infiltrating (7) and circulating (8) CD8+ T cells exhibit metabolic insufficiency, characterized most prominently by persistent loss of mitochondrial function and mass (7), typically following progressive loss of peroxisome proliferator-activated receptor γ coactivator 1α (PGC-1α) (7).
Molecular hydrogen, that is dihydrogen or H2, was previously reported to efficiently neutralize hydroxyl radicals (•OH), but not other reactive oxygen species, including superoxide anions (O2•−), hydrogen peroxide (H2O2) and nitric oxide (NO•) (9). Accordingly, hydrogen is now believed to reduce oxidative stress and ischemia-reperfusion injury in the brain, spinal cord (10), myocardium (11), intestinal epithelium (12), retina, testes (13) and kidneys (14). Hydrogen has been used to treat various states associated with oxidative stress, including trauma (15), neurodegenerative disease (16), inflammatory disease (17), organ transplantation, metabolic syndrome (18), diabetes mellitus (19), sepsis (20), burns (21), adverse reactions to chemotherapy (22), radiation injury (23), hearing disorders and preeclampsia (24). There are several studies on the preventive and therapeutic effects of hydrogen on various diseases, including cancer (25–27). Notably, it was reported that molecular hydrogen activates PGC-1α (28), which is a positive regulator of mitochondrial biogenesis and respiration, adaptive thermogenesis, gluconeogenesis and a number of other metabolic processes (29), suggesting that it may rescue exhausted CD8+ T cells with mitochondrial dysfunction.
Therefore, the present study investigated whether PD-1 expression in circulating CD8+ T cells in 55 patients with colorectal carcinoma was associated with progression-free survival (PFS) and overall survival (OS), and whether hydrogen gas impacts prognosis via influencing PD-1+ CD8+ T lymphocytes.
Materials and methods
Patients, sample collection and processing
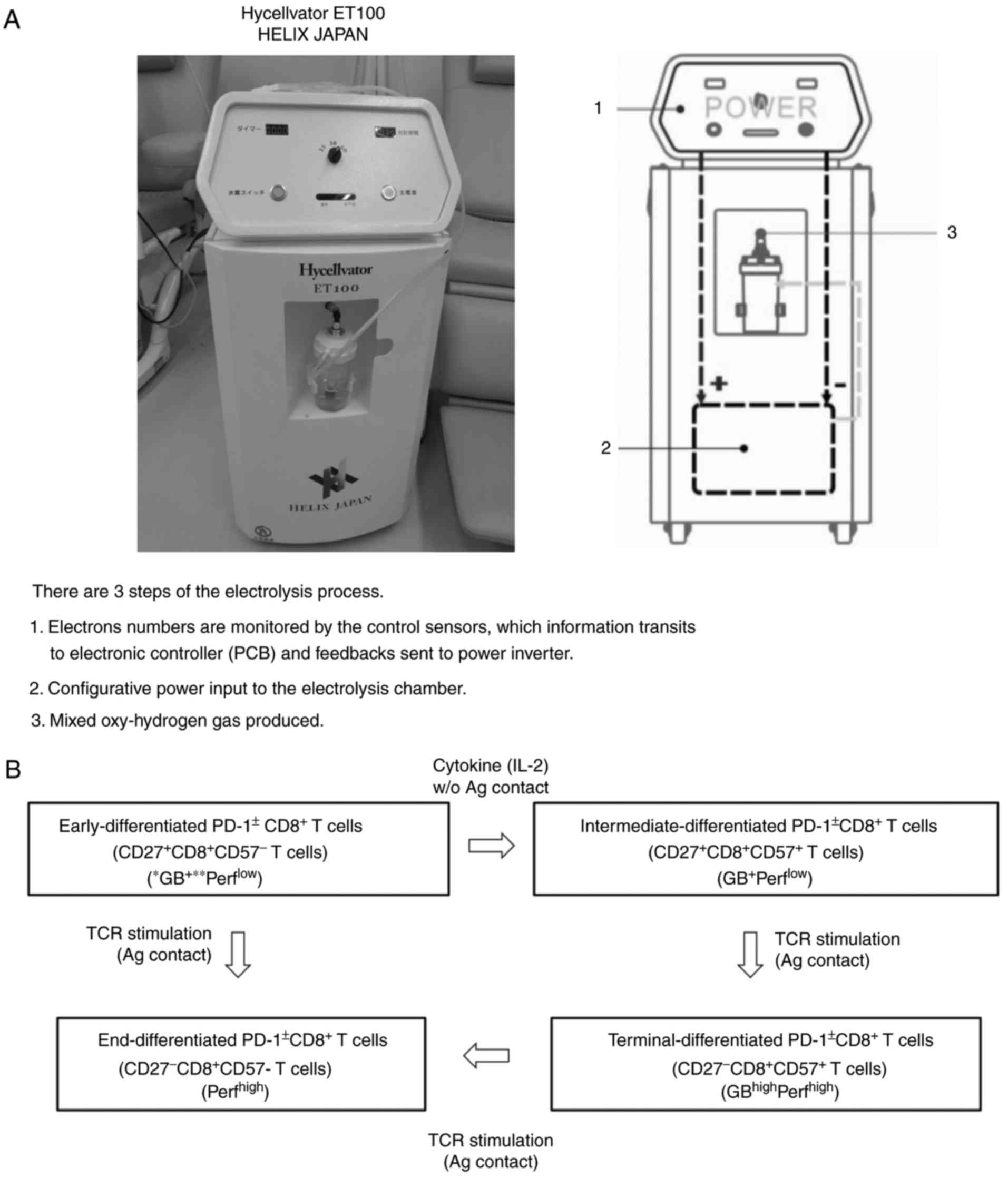
All participants provided written informed consent prior to enrollment, and the Institutional Review Boards at the Tamana Regional Health Medical Center (Tamana, Kumamoto, Japan) approved the study protocol. All methods and procedures were consistent with Good Clinical Practice, the Declaration of Helsinki and local laws. In total, 55 patients with histologically and clinically diagnosed stage IV colorectal carcinoma, based on the unified Tumor-Node-Metastasis criteria (30), were enrolled at Tamana Regional Health Medical Center between July 2014 and July 2017. The specific inclusion and exclusion criteria were a performance status of ≥2 and <2, respectively. Among the patients with colorectal carcinoma, there were 21 men and 34 women, who ranged in age from 28 to 96 years, with a mean age of 65.7±14.8 years (Table I). The patients were treated with chemotherapy using XELOX (CapeOX) (1,200-1,800 mg capecitabine for 14 days continuously, followed by a 7-day rest period, and 85 mg/m2 oxaliplatin at a 3-week interval) + bevacizumab (7.5 mg/m2 at a 3-week interval). A total of 3 weeks was regarded as one cycle. Treatment was repeated until the cancer progression was confirmed by imaging. The patients inhaled hydrogen gas for 3 h daily at their own homes through a cannula or mask, rented or purchased by themselves, connected to a Hycellvator ET 100 (Helix Japan, Co., Ltd., Tokyo, Japan) (Fig. 1A). None of the patients reported any complaints regarding the daily 3-h hydrogen gas inhalation. Peripheral blood (10 ml) was collected from the patients prior to and 3 months after treatment with hydrogen gas.
Figure 1.
(A) Hycellvator ET100 (Helix Japan, Co., Ltd.), which generates hydrogen gas. (B) Differentiation pathway of CD8+ T cells from early-differentiated to end-differentiated CD8+ T cells (via intermediate- and terminal-differentiated CD8+ T cells). PCB, printed circuit board; CD, cluster of differentiation; GB, granzyme; Perf, perforin.
Table I.
Comparison of clinicopathological data between patients with high- and low-terminal PD-1+ CD8+ T cells.
Hydrogen gas treatment
The Hycellvator ET 100 (Helix Japan, Co., Ltd.) generates 1.67 l/min hydrogen gas (hydrogen purity, 99.99%) by electrolysis. As measured by gas chromatography at Kureha Special Laboratory (Iwaki, Fukushima, Japan), the gas generated consisted of 680,000 ppm hydrogen gas and 320,000 ppm oxygen gas. Recently, hydrogen gas inhalation was used in patients with post-cardiac arrest syndrome, and adverse events were not observed (31). Furthermore, no adverse events were observed in the 55 patients who inhaled hydrogen gas for 3 months in the present study.
Antibodies and fluorescence-activated cell sorting (FACS)
Briefly, Ficoll-Hypaque solution (20 ml) was placed into a 50-ml conical centrifuge tube using a sterile pipette. Anti-coagulated blood (10 ml) mixed with an equal volume of PBS was then slowly layered over the Ficoll-Hypaque solution by gently pipetting down the side of the tube. Subsequently, samples were centrifuged for 40 min at 400 × g and 22°C for 30–40 min with no braking. Mononuclear cells that accumulated at the interface between the plasma (upper) and Ficoll-Hypaque layers (bottom) were carefully recovered using a Pasteur pipette and transferred to a 15-ml conical tube. Cells were then analyzed on a BD FACSCalibur (Nippon Becton Dickinson, Tokyo, Japan) with BD CellQuest software (version 5.1), using anti-CD57 conjugated to fluorescein isothiocyanate (clone NK-1; cat. no. 347393; Nippon Becton Dickinson), mouse anti-human CD27 conjugated to APC (clone M-T271; cat. no. B09983; Beckman Coulter, Tokyo, Japan), mouse anti-human PD-1 conjugated to PE (clone EH12.1; cat. no. 557946; Nippon Beckton Dickinson) and mouse anti-human CD8 conjugated to PerCP (clone SK1; cat. no. 347314) (BD Pharmingen, San Jose, CA, USA), incubated at 4°C for 30 min, following blocking with 1% γ-globulin for 15 min at 4°C. To determine the independent contributions of each marker to PFS and OS, FACS data were used to stratify patients based on the proportion of early, intermediate, terminal, and end PD-1+ and PD-1− CD8+ T cells. All blood samples obtained from the patients were transferred to SRL, Inc. (Tokyo Japan), where lymphocyte separation and flow cytometry were performed. Therefore, the status of the laboratory data, reliable protocols and flow cytometry assays were certified by SRL, Inc., one of the most reliable clinical laboratory centers in Japan. The flow cytometry data was analyzed using SPSS version 19.0 for Windows (IBM Corp., Armonk, NY, USA).
Study endpoints and assessments
The primary endpoints were PFS and OS time, which were measured from the date of randomization to the first recurrence and mortality regardless of cause, respectively. Patients were monitored by dynamic computed tomography or magnetic resonance imaging every 3 months from the baseline up to 60 months and every 3–6 months thereafter. Two independent and blinded radiologists, each with >5 years of experience, reviewed all scans at each site. In cases of discord, the two radiologists reviewed the images to reach the same conclusion following discussion. Adverse events were classified and graded every 2 months according to the Common Terminology Criteria for Adverse Events version 3.0 (National Cancer Institute, Bethesda, MD, USA) (32) from the day of consent until the end of the study at least 30 days after the treatment. Multiple events were counted once for each patient, of which the most severe was noted.
Statistical analysis
Testing of the significance of the differences between groups was performed using the χ2 test. In case of persistent abnormal distribution, the linear correlation between two continuous variables was tested with the Spearman correlation coefficient. Receiver operating characteristic (ROC) analysis was used to determine optimal cut-off values for continuous variables. The ROC curve shows 1-specificity on the x-axis and sensitivity on the y-axis. The optimal cut-off value is calculated by maximizing the sensitivity and specificity across various cut-off points on the ROC curve. The probability of survival was estimated by the Kaplan-Meier method, and differences in survival were evaluated by the log-rank test. Prognostic factors were tested by univariate and multivariate Cox regression. All statistical analyses were performed using SPSS version 19.0 for Windows (IBM Corp.). Differences were considered statistically significant at P<0.05.
Results
Circulating terminal PD-1+ CD8+ T cells are critical for prognosis in colorectal cancer
In the normal state, early CD8+ T cells abundantly express PD-1, which gradually diminishes with differentiation into terminal CD8+ T cells. However, loss of PD-1 is delayed in patients with cancer and may result in a poor prognosis. Hence, Cox proportional-hazards regression analysis was used to identify PD-1+/− CD8+ T cell subsets (Fig. 1B) and clinicopathological factors [age, sex, primary tumor (T), regional lymph nodes (N), distant metastasis (M) and histology] associated with PFS and OS in patients with stage IV colorectal cancer. By univariate analysis of 18 factors, including 6 clinicopathological factors, terminal PD-1+ CD8+ T cells were found to be significantly associated with poorer PFS [hazard ratio (HR), 1.239; 95% confidence interval (CI), 1.106–1.389; P<0.0001] and OS (HR, 1.183; 95% CI, 1.066–1.314; P=0.002), as were end PD-1+ CD8+ T cells (PFS: HR, 1.296; 95% CI, 1.053–1.595; P=0.015; OS: HR, 1.333; 95% CI, 1.103–1.610; P=0.003). By contrast, early PD-1− and end PD-1− CD8+ T cells were associated with better (HR, 0.961; 95% CI, 0.926–0.997; P=0.036) and worse (HR, 1.044; 95% CI, 1.005–1.084; P=0.025) OS, respectively. The univariate analysis data of the other 14 factors for PFS and OS, respectively, were as follows: Age, P=0.270 and P=0.886; sex, P=0.894 and P=0.398; T factor, P=0.332 and P=0.664; N factor, P=0.080 and P=0.150; M factor (the univariate analysis could not be performed as all patients had distant metastasis); histology, P=0.503 and P=0.184; early CD8+ T cells, P=0.953 and P=0.273; early PD-1+ CD8+ T cells, P=0.757 and P=0.560; intermediate CD8+ T cells, P=0.434 and P=0.560; intermediate PD-1+ CD8+ T cells P=0.799 and P=0.505; intermediate PD-1− CD8+ T cells P=0.137 and P=0.099; terminal CD8+ T cells, P=0.453 and P=0.595; terminal PD-1− CD8+ T cells, P=0.681 and P=0.886; and end CD8+ T cells, P=0.285 and P=0.566.
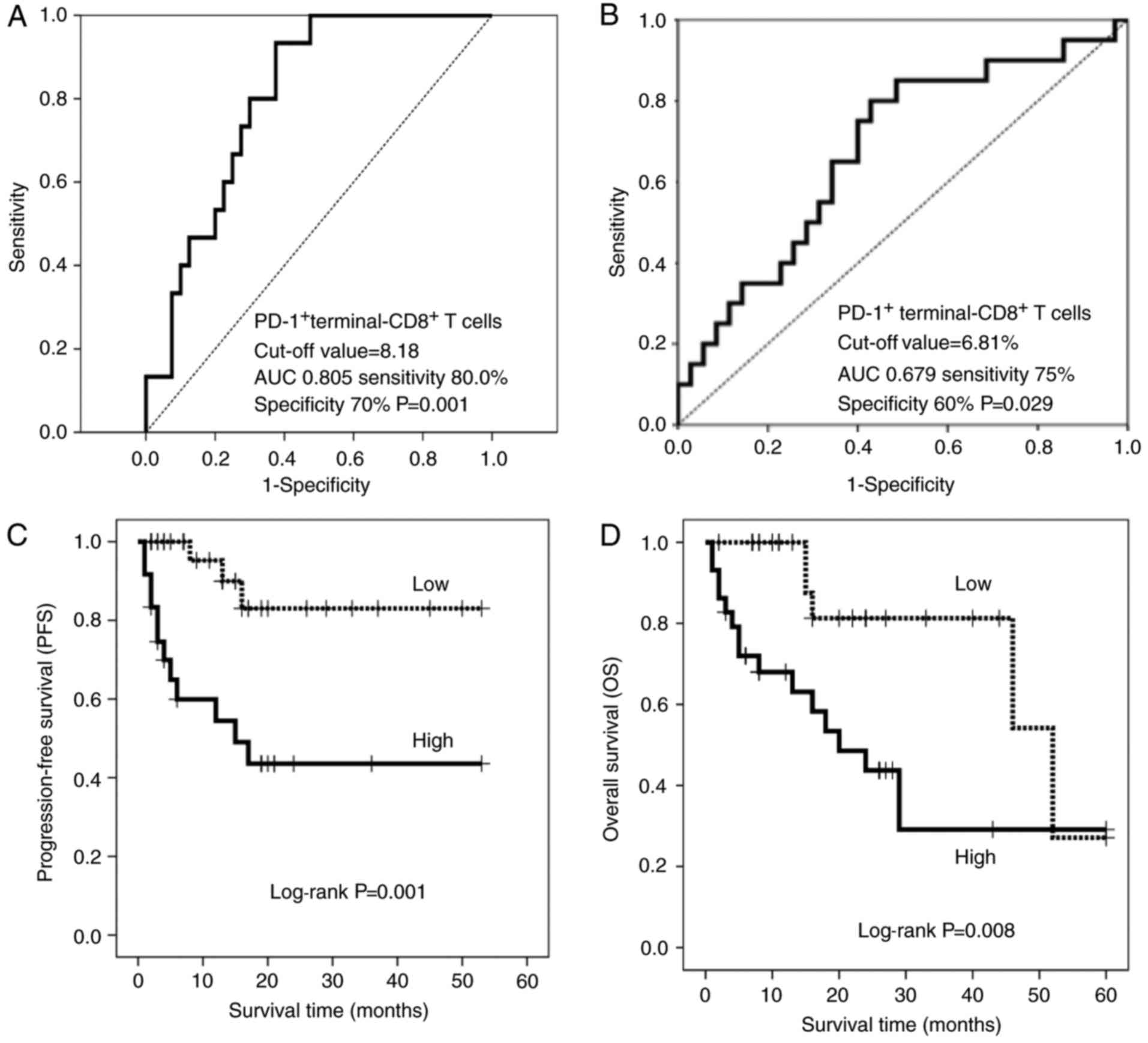
Based on multivariate Cox regression, terminal PD-1+ CD8+ T cells were more strongly associated with PFS (HR, 1.239; 95% CI, 1.106–1.389; P<0.0001) and OS (HR, 1.136; 95% CI, 1.019–1.266; P=0.022) than others. The multivariate data of the other 3 factors were as follows: Early PD-1− CD8+ T cells, P=0.677 for PFS and P=0.352 for OS; end PD-1+ CD8+ T cells, P=0.274 for PFS; HR, 1.247; 95% CI, 1.007–1.543; P=0.043; and end PD-1− CD8+ T cells, P=0.561 for PFS and P=0.206 for OS). Accordingly, patients were stratified based on the abundance of terminal PD-1+ CD8+ T cells, using cut-off values of 8.18 and 6.81% for PFS and OS, respectively, as determined from receiver operating characteristic curves (Fig. 2A and B). There were no significant differences in clinicopathological factors between the patients with high and low terminal PD-1+ CD8+ T cells (Table I). The resulting stratified Kaplan-Meier survival curves revealed that PFS (log-rank test, P=0.001) and OS (log-rank test, P=0.008) were significantly worse for patients with terminal PD-1+ CD8+ T cells higher than the cut-off (Fig. 2C and D). The median PFS time was 18 months for the patients with a high-terminal PD-1+ CD8+ T cell ratio, but was not reached (>50% of patients remained alive) for those with a low-terminal PD-1+ CD8+ T cell ratio, while OS was 18 months for the patients with a high-terminal PD-1+ CD8+ T cell ratio and 46 months for those with a low-terminal PD-1+ CD8+ T cell ratio.
Figure 2.
Receiver operating characteristic curves of (A) PFS and (B) OS based on terminal PD-1+ CD8+ T cells. The cut-off values are 8.18 and 6.81%, respectively. (C) PFS and (D) OS in patients with a high- (solid line) and low- (dotted line) percentage of terminal PD-1+ CD8+ T cells. PFS, progression-free survival; OS, overall survival; AUC, area under the curve; PD-1, programmed cell death 1; CD, cluster of differentiation.
Hydrogen gas reduces the proportion of PD-1+ CD8+ T cells and improves prognosis
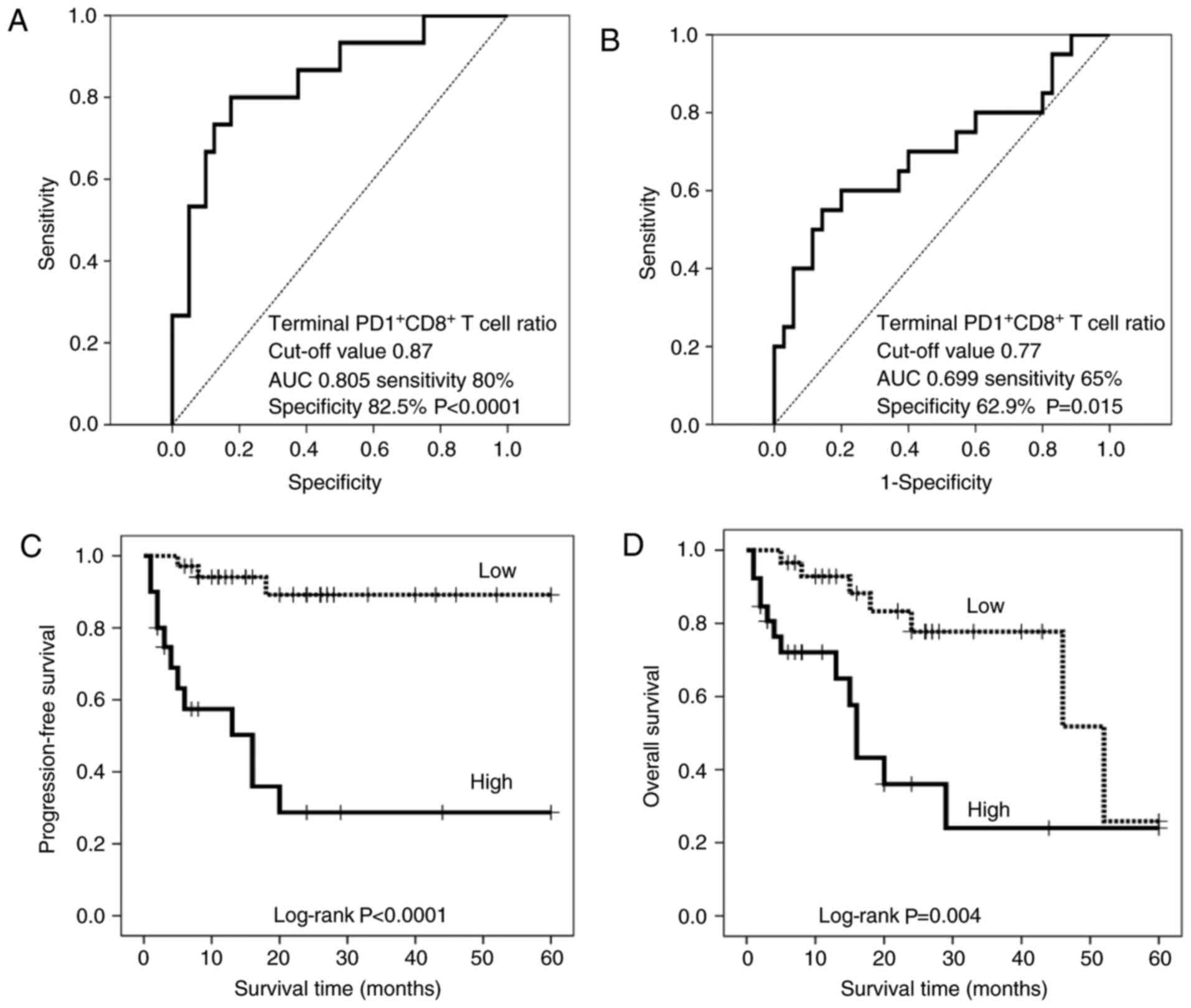
Molecular hydrogen was reported to activate PGC-1α (28), which enhances mitochondrial activity (29), thereby rescuing exhausted CD8+ T cells with inactive mitochondria following progressive loss of PGC-1α (15). Therefore, the present study investigated whether hydrogen gas alters the proportion of PD-1+/− CD8+ T cell subsets and whether alterations, if any, are associated with prognosis in patients with stage IV cancer. Notably, hydrogen gas reduced the proportion of early, intermediate, terminal and end PD-1+ CD8+ T cells in 27 (49.1%), 28 (50.9%), 35 (63.6%) and 32 (58.2%) out of 55 patients, respectively. Conversely, hydrogen gas enhanced the proportion of early, intermediate, terminal and end PD-1− CD8+ T cells in 32 (58.2%), 27 (49.1%), 39 (70.9%) and 31 (56.4%) patients, respectively. Univariate analysis showed that the ratio of the proportion of intermediate PD-1+ CD8+ T cells following treatment with hydrogen gas to that prior to treatment (intermediate PD-1+ CD8+ T cell ratio) was significantly associated with shorter PFS (HR, 2.286; 95% CI, 1.284–4.070; P=0.005) and OS (HR, 2.398; 95% CI, 1.384–4.156; P=0.002) times. Similar associations were observed for the intermediate PD-1− CD8+ T cell ratio (PFS: HR, 2.286; 95% CI, 1.284–4.070; P=0.005; OS: HR, 2.398; 95% confidence interval, 1.384–4.156; P=0.002) and terminal PD-1+ CD8+ T cell ratio (PFS: HR, 6.459; 95% CI, 2.384–17.50; P<0.0001; OS: HR, 4.158; 95% CI, 1.718–10.06; P=0.002). By contrast, the early PD-1− CD8+ T cell ratio was predictive of worse OS time (HR, 2.398; 95% CI, 1.384–4.156; P=0.002), whereas the terminal PD-1− CD8+ T cell ratio was significantly associated with increased overall survival time (HR, 0.002; 95% CI, 0.000–0.131; P=0.004). For the multivariate analysis, the terminal PD-1+ CD8+ T cell ratio was found to be an independent predictor of poor PFS (HR, 6.459; 95% CI, 2.384–17.50; P<0.0001) and OS (HR, 2.957; 95% CI, 1.185–7.378; P=0.020). Based on these results, patients were stratified as having a high and low terminal PD-1+ CD8+ T cell ratio using cut-off values of 0.87 and 0.77% for PFS and OS, respectively (Fig. 3A and B). There were no significant differences in clinicopathological factors between the patients with high and low terminal PD-1+ CD8+ T cell ratio (Table II). The resulting stratified PFS and OS curves are plotted in Fig. 3C and D, and show that patients with a low terminal PD-1+ CD8+ T cell ratio have significantly increased PFS (P<0.0001) and OS (P=0.004) times compared with those with high ratios. The median follow-up time was 13 months for the patients with a high-terminal PD-1+ CD8+ T cell ratio, but was not reached (>50% of patients remained alive) for those with a low-terminal PD-1+ CD8+ T cello ratio, while that of OS was 15 months for the patients with a high-terminal PD-1+ CD8+ T cell ratio and 46 months for those with a low-terminal PD-1+ CD8+ T cell ratio.
Figure 3.
Analysis of the ratio of terminal PD-1+/− CD8+ T cells prior to and following treatment with hydrogen gas (terminal PD-1+/− CD8+ T cell ratio). Receiver operating characteristic curve of (A) PFS and (B) OS based on the terminal PD-1+ CD8+ T cell ratio. The cut-off values are 0.87 and 0.77%, respectively. (C) PFS and (D) OS in patients with a high-(solid line) and low-(dotted line) terminal PD-1+ CD8+ T cell ratio. PFS, progression-free survival; OS, overall survival; AUC, area under the curve; PD-1, programmed cell death 1; CD, cluster of differentiation.
Table II.
Comparison of clinicopathological data between patients with high- and low-terminal PD-1+ CD8+ T cell ratio (the ratio of terminal PD-1+ CD8+ T cells following the hydrogen treatment to prior to it).
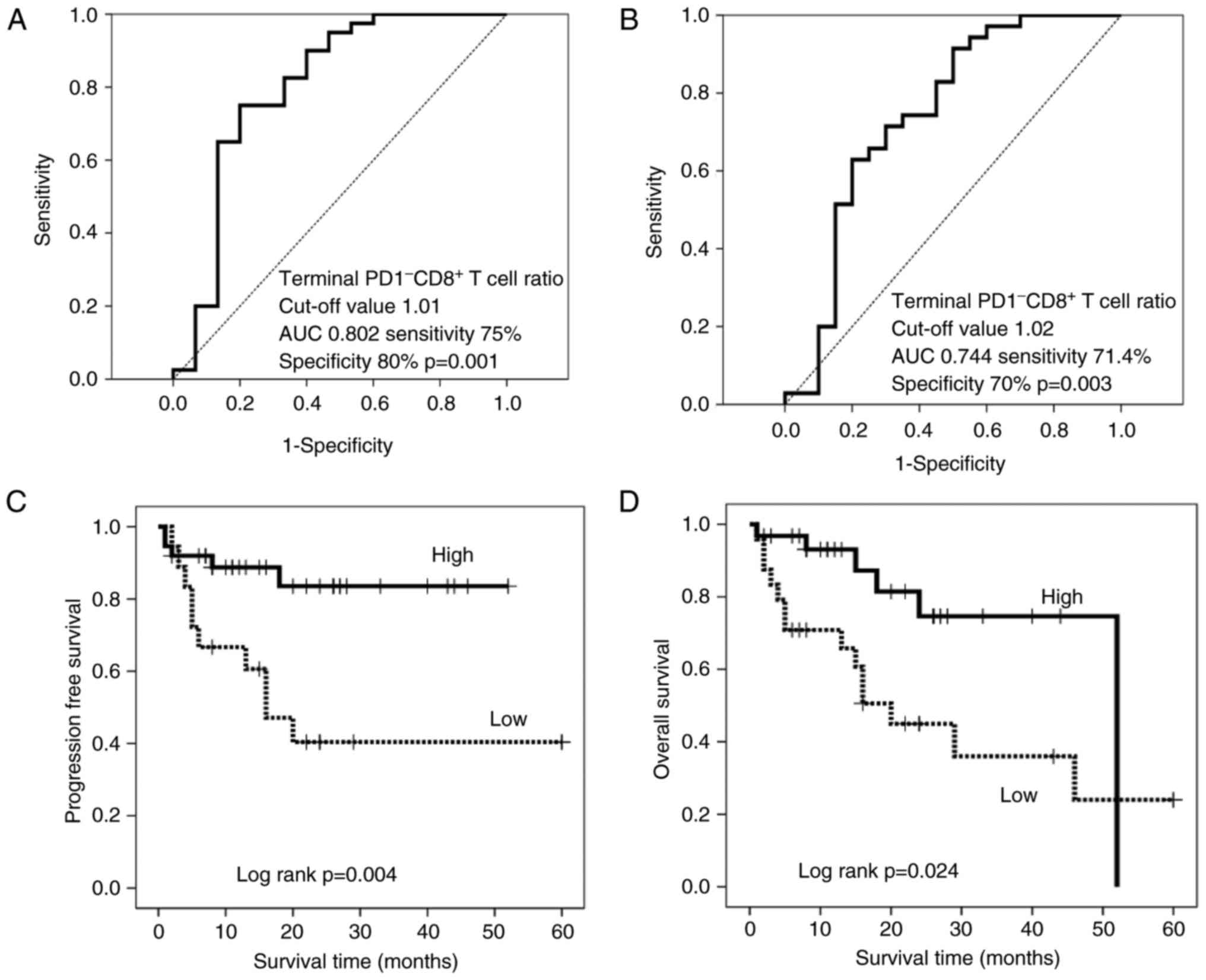
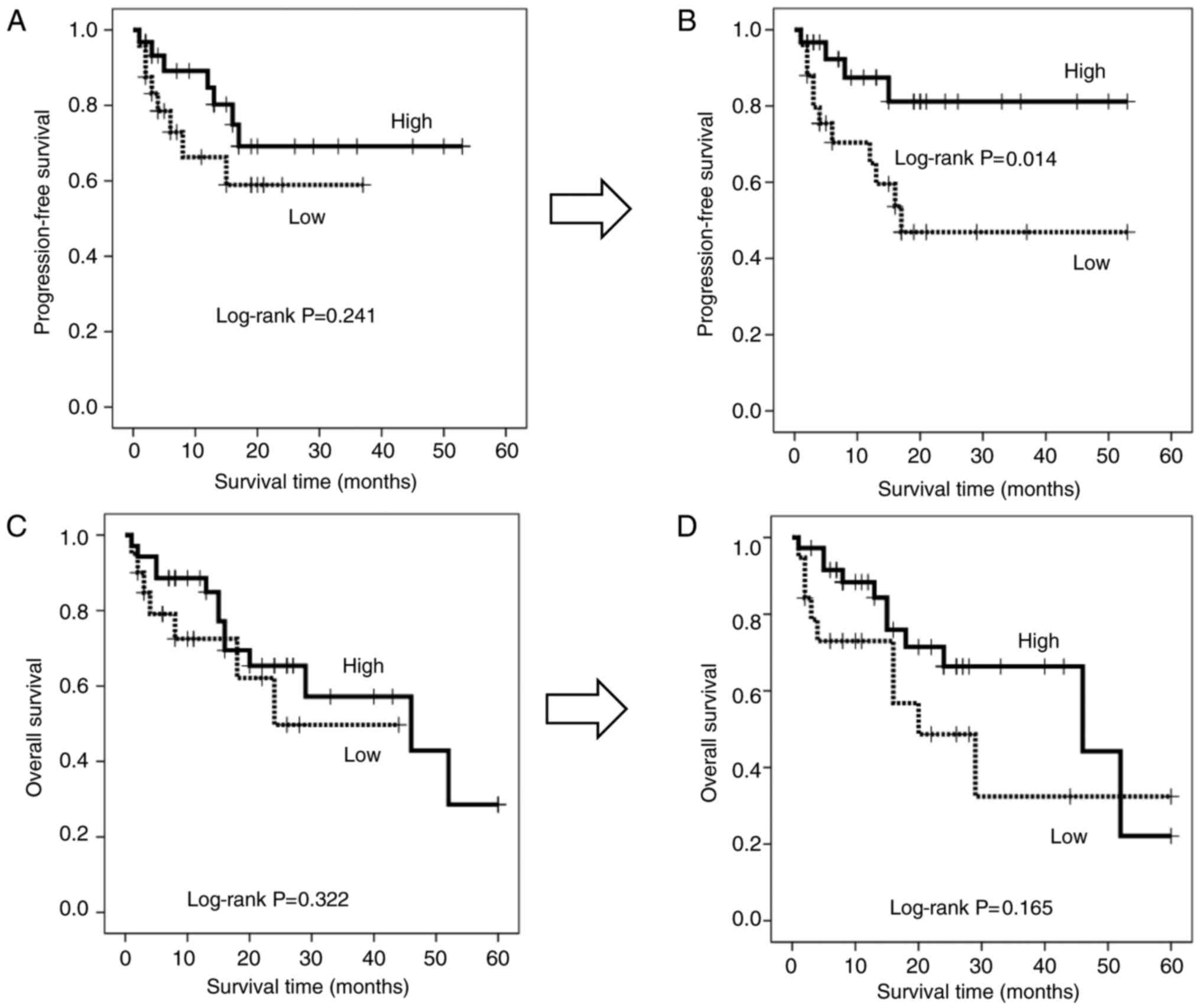
Hydrogen-induced accumulation of terminal PD-1− CD8+ T cells is associated with an improved prognosis
Based on the hypothesis that hydrogen gas may activate mitochondrial function and thereby convert exhausted terminal PD-1+ CD8+ T cells into active terminal PD-1− CD8+ T cells, the present study investigated whether the change in the abundance of the latter impacts prognosis in patients treated with hydrogen gas. Thus, patients were stratified by the terminal PD-1− CD8+ T cell ratio based on cut-off values of 1.01 and 1.02 for PFS (Fig. 4A) and OS (Fig. 4B), respectively. There were no significant differences in clinicopathological factors between the patients with high- and low-terminal PD-1− CD8+ T cell ratios (Table III). The resulting stratified survival curves are plotted in Fig. 4C and D, respectively, and indicate that patients with high ratios have significantly increased PFS (P=0.004) and OS (P=0.024) times compared with those with low ratios. The median follow-up time was 15 months for the patients with a low-terminal PD-1− CD8+ T cell ratio, but was not reached (>50% of patients remained alive) for those with a high-terminal PD-1− CD8+ T cell ratio, while that of OS was 16 months for the patients with a low-terminal PD-1− CD8+ T cell ratio and 52 months for those with a high-terminal PD-1− CD8+ T cell ratio. Furthermore, hydrogen gas treatment resulted in a significantly longer PFS time (P=0.014) and a generally longer, but non-significant, OS time (P=0.165) in patients with a high level of terminal PD-1− CD8+ T cells compared with that in patients with a low level, although there was no significant difference between the groups prior to treatment (Fig. 5A and C).
Figure 4.
Receiver operating characteristic curve of (A) PFS and (B) OS based on the terminal PD-1− CD8+ T cell ratio, with cut-off values of 1.01 and 1.02%, respectively. (C) PFS and (D) OS in patients with a high- (solid line) and low- (dotted line) terminal PD-1− CD8+ T cell ratio. PFS, progression-free survival; OS, overall survival; AUC, area under the curve; PD-1, programmed cell death 1; CD, cluster of differentiation.
Figure 5.
Progression-free survival in patients with a high-(solid line) and low-(dotted line) terminal PD-1− CD8+ T cell ratio (A) prior to and (B) following treatment with hydrogen gas. Comparison of overall survival between patients with a high-(solid line) and low-(dotted line) terminal PD-1− CD8+ T cell ratio (C) prior to and (D) following treatment with hydrogen gas. PD-1, programmed cell death 1; CD, cluster of differentiation.
Table III.
Comparison of clinicopathological data between patients with high- and low-terminal PD-1− CD8+ T cell ratio.
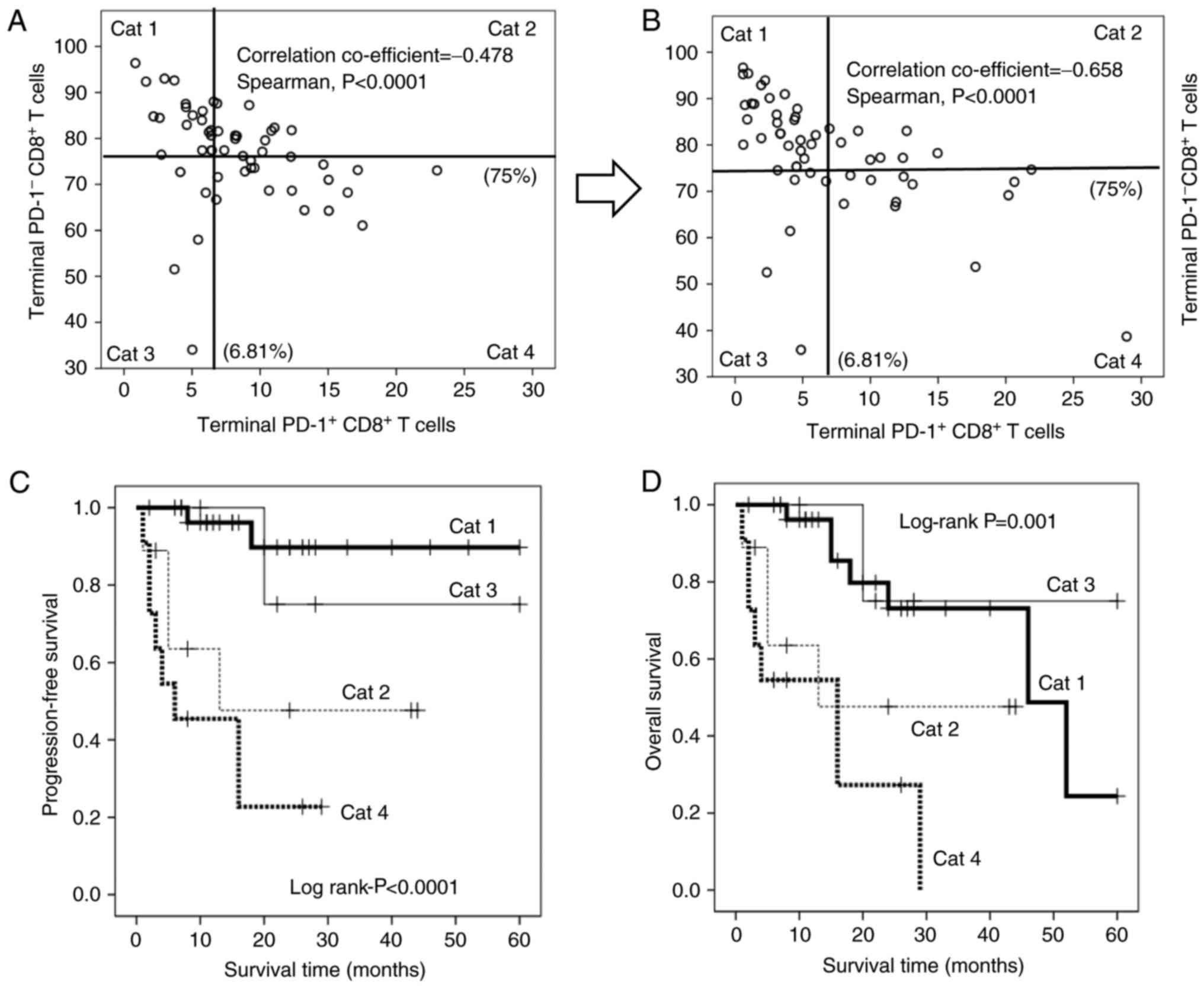
Serum terminal PD-1+/− CD8+ T cells are important immune indices in patients with advanced cancer
As aforementioned, hydrogen gas reduces the proportion of terminal PD1+ CD8+ T cells, but increases the abundance of terminal PD1− CD8+ T cells, and the magnitude of these changes is strongly associated with the prognosis. Notably, the terminal PD1+ CD8+ T cells were significantly and inversely correlated with the terminal PD1− CD8+ T cells (Fig. 6A and B), suggesting that the dynamic balance between these subsets contributes strongly to prognosis in patients with advanced colorectal carcinomas. Therefore, patients were stratified based on all possible high/low combinations of these subsets [category (Cat) 1–4; Cat 1: Patients with low PD1+ and high PD1− terminal CD8+ T cells; Cat 2: Patients with high PD1+ and high PD1− terminal CD8+ T cells; Cat 3: Patients with low PD1+ and low PD1− terminal CD8+ T cells; Cat 4: Patients with high PD1+ and high PD1− terminal CD8+ T cells; Fig. 6A and B]. Kaplan-Meier analysis revealed that Cat 1 patients experienced significantly longer PFS times than all other groups, whereas Cat 3 patients experienced significantly longer OS times than the others. By contrast, Cat 4 patients experienced significantly worse PFS (Fig. 6C) and OS (Fig. 6D) times than others. Hydrogen gas also increased the number of patients with low PD1+ terminal CD8+ T cells (Cat 1 and 3), but decreased the number of patients with high PD1+ terminal CD8+ T cells (Cat 2 and 4), leading to an improved prognosis in patients with stage IV colorectal carcinoma (Fig. 6A and B; Table IV).
Figure 6.
Point diagram of the correlation between terminal PD-1+ (x-axis) and PD-1− CD8+ T cells (y-axis) (A) prior to and (B) following treatment with hydrogen gas. The x-axis of terminal PD-1+ and the y-axis of PD-1− CD8+ T cells are divided into two sections with cut-offs of 6.81 and 75%, respectively. Cat 1: Low-terminal PD-1+ CD8+ T cells and high-terminal PD-1− CD8+ T cells; Cat 2: High-terminal PD-1+ CD8+ T cells and high-terminal PD-1− CD8+ T cells; Cat 3: Low-terminal PD-1+ CD8+ T cells and low-terminal PD-1− CD8+ T cells; Cat 4: High-terminal PD-1+ CD8+ T cells and low-terminal PD-1 CD8+ T cells. (C) Progression-free survival and (D) overall survival in Cat 1 (bold line), Cat 2 (thin dotted line), Cat 3 (thin line) and Cat 4 (bold dotted line) patients. PD-1, programmed cell death 1; CD, cluster of differentiation; Cat, category.
Table IV.
Change of category following hydrogen gas treatment.
Discussion
Persistent stimulation by carcinoma cells renders cytotoxic CD8+ T cells into an exhausted state without proliferation, cytokine production or cytotoxic capabilities. Accumulation of exhausted CD8+ T cells in the peripheral blood, as well as at the tumor site, has been reported to result in a poor prognosis in patients with cancer (3–6). In the present study, terminal PD-1+ CD8+ T cells were an independent poor prognostic factor in the patients with stage IV colorectal carcinoma. It was recently reported that exhausted CD8+ T cells exhibit mitochondrial dysfunction, caused by the inactivation of PGC-1α, to express immune checkpoint inhibitors such as PD-1 and Tim-3, but return to the active effector state following exposure to certain stimulants (7). Hydrogen was recently reported to stimulate PGC-1α (28), which enhances mitochondrial function (29) and thus may rescue exhausted CD8+ T cells. The present study found that hydrogen gas reduced the proportion of all four PD-1+ CD8+ T cell subsets and increased the proportions of all four PD-1− CD8+ subsets. Univariate and multivariate analyses indicated that loss of terminal PD-1+ CD8+ T cells is the most significant contributor to improved prognosis. Furthermore, reduction of terminal PD-1+ CD8+ T cells and accumulation of terminal PD-1− CD8+ T cells following hydrogen gas treatment were significantly associated with improved PFS (Figs. 3C and 4C) and OS (Figs. 3D and 4D) times. Moreover, treatment with hydrogen gas significantly extended PFS time in patients with abundant PD-1− CD8+ T cells compared with time in others (Fig. 5B) and slightly improved OS, although this result was not significant (Fig. 5D). Collectively, these results suggested that hydrogen gas converts exhausted terminal PD-1+ CD8+ T cells into active terminal PD-1− CD8+ T cells, thereby improving prognosis.
The present study found that circulating terminal PD-1+ CD8+ T cells in patients with stage IV colorectal cancer were strongly and independently associated with short PFS and OS times, in agreement with recent reports that circulating and tumor-infiltrating PD-1+ CD8+ T cells contribute to poor prognosis in various cancer types, including breast, pancreatic and gastric cancer (7–10). These results suggested that prognosis and therapeutic response in patients with cancer may be easily and non-invasively predicted based on terminal PD-1+ CD8+ T lymphocytes in the peripheral blood, consistent with data demonstrating that circulating CD8+ PD-1+ lymphocytes could provide a window into determining the characteristics of tumor-resident antitumor lymphocytes (8). The abundance of terminal PD-1+ CD8+ T cells was inversely correlated with that of terminal PD-1− CD8+ T cells (Fig. 6A and B), and a novel classification system composed of four quadrants was created (Fig. 6). The patients belonging to the first (Cat 1) and third (Cat 3) quadrants, in whom the proportion of terminal PD-1+ CD8+ T cells was below the cut-off value, had an improved prognosis (Fig. 6C and D). By contrast, the patients belonging to the second (Cat 2) and fourth (Cat 4) quadrants, who had a higher level of terminal PD-1+ CD8+ T cells than the cut-off value had a poorer prognosis, particularly the patients of Cat 4, with the worst PFS and OS times (Fig. 6C and D). These results suggested that the balance between terminal PD-1+ and PD-1+ CD8+ T cells is critical for cancer prognosis and that the novel patient classification system based on terminal PD-1+ and PD-1− CD8+ T cells is useful to predict therapeutic effects, as well as prognosis.
In the future, in order to confirm that hydrogen gas can restore exhausted CD8+ T cells (PD-1+ CD8+ T cells) into active CD8+ T cells (PD-1− CD8+ T cells) by the activation of the mitochondria, we will investigate whether the aforementioned conversion (PD-1+ CD8+ T cells → PD-1− CD8+ T cells) is associated with measured values of coenzyme Q10 (CoQ10) and growth differentiation factor 15 (GDF15), which are supposed to reflect actual mitochondrial function. Tim-3, a member of the recently discovered T cell Immunoglobulin and mucin domain family, is supposed to be expressed on senescent CD8+ T cells, of which mitochondrial function may be irreversible (33). CoQ10 and GDF15 will also be measured on senescent CD8+ T cells (Tim-3+ CD8+ T cells). Furthermore, future studies will investigate whether hydrogen gas actually converts PD-1+ CD8+ T culture cells into PD-1− CD8+ T culture cells in vitro.
In conclusion, hydrogen gas decreases the number of terminal PD-1+ CD8+ T cells, i.e., exhausted CD8+ T cells, possibly by activating mitochondria via PGC-1α, thereby increasing the number of terminal PD-1− CD8+ T cells and improving the patient prognosis. Thus, terminal PD-1+ and PD-1− CD8+ T cells are critical immune parameters in patients with cancer and are conveniently measurable in the peripheral blood. A novel system for patient classification (Cat 1–4) based on these indices was also developed in the present study in order to assist in predicting prognosis and therapeutic response.
Acknowledgements
The authors would like to thank Helix Japan, Co., Ltd. (Tokyo, Japan) for providing the Hycellvator ET 100 hydrogen gas generator.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Authors’ contributions
JA was involved in the analysis and interpretation of the data, and HB was involved in the analysis of the data. All authors read and approved the final manuscript.
Ethics approval and consent to participate
All procedures performed in studies involving human participants were approved and in accordance with the ethical standards of Kumamoto University (Kumamoto, Japan) and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study.
Patient consent for publication
Approval was obtained from all patients for the publication of the study.
Competing interests
The authors declare that they have no conflicts of interest.
Glossary
Abbreviations
Abbreviations:
FACS fluorescence-activated cell sorting
PD-1 programmed cell death 1
PGC-1α peroxisome proliferator-activated receptor γ coactivator 1α
PFS progression-free survival
OS overall survival
| |
| |
| |
| |
| |
| |
| |
| |
| |
| |
| |
| |
| |
| |
| |
| |
| |
| |
| |
| |
| |
| |
| |
| |
| |
| |
| |
| |
| |
| |
| |
| |
|